Experts say improved access to lung cancer screening critical to saving lives across Asia
Urgent shift to low-dose CT screening recommended
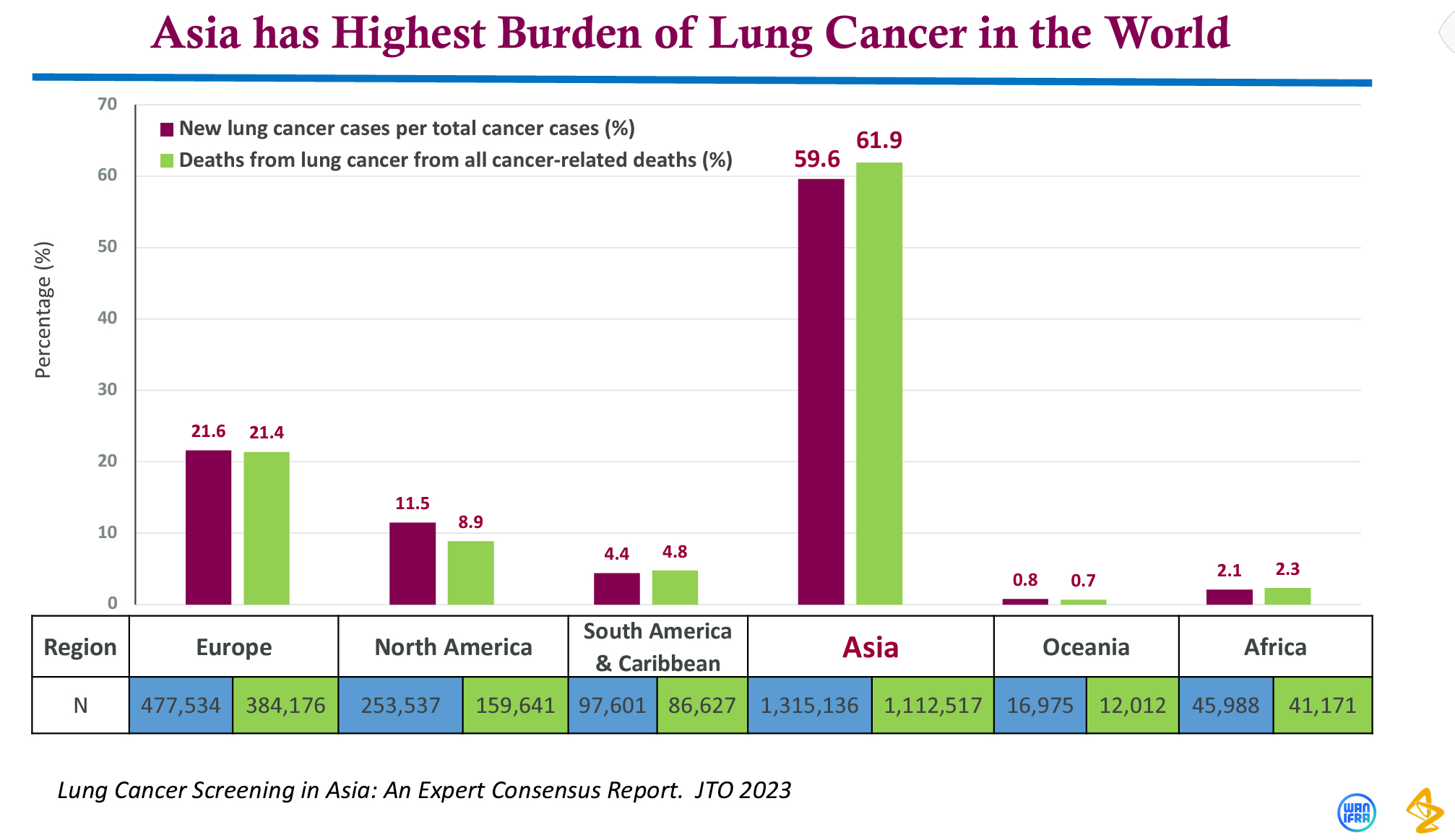
SINGAPORE—Lung cancer kills more people in Asia than anywhere else in the world, but a consensus reached by 19 experts from across Asia suggests that deaths from the disease could be decreased by ensuring earlier diagnosis through improved screening access and modifications to screening procedures.
The consensus is the result of extensive discussion among experts from Hong Kong, India, Indonesia, Japan, Malaysia, Philippines, Singapore, South Korea, Taiwan, Thailand, and Vietnam, as supported by the Lung Ambition Alliance (LAA), a non-profit collaboration of the International Association for Study of the Lung Cancer, Global Lung Cancer Coalition, AstraZeneca, and Guardant Health.
Experts recommended shifting from traditional chest X-rays to a more advanced procedure known as low-dose computed tomography (LDCT), which uses a computer and low dose X-rays to generate a series of images and can help detect lung abnormalities such as tumors.
“The expert concensus calls for urgent changes to initiate low-dose computed tomography (LDCT) screening programs for people who could be at risk of lung cancer across Asia. This is important to introduce more sensitive screening across the region and drive earlier detection of lung cancer, when there is a greater potential for cure,” Dr. Pan-Chyr Yang, chair professor of the National Taiwan University’s College of Medicine, said in a media briefing on the sidelines of the 2023 World Conference on Lung Cancer.
Yang pointed out that the LAA hopes to reduce lung cancer as a cause of death, with the first goal of doubling the five-year survival rate for lung cancer patients by 2023.
Lower mortality rate
A US clinical trial involving over 50,000 participants found a 20 percent reduction in lung cancer deaths with LDCT screening compared to chest X-rays due to improved early cancer detection.
Yang emphasized that the changes will significantly protect lives in Asia, where three in five cases of lung cancer occur, affecting over 1.3 million patients.
Furthermore, the consensus has shown that patients with detected screening abnormalities during routine health screening and persistent exposure to risk factors should be screened with LDCT once a year, while high-risk heavy smokers should be screened twice a year.
In most parts of Asia, including the Philippines, LDCT is still not implemented in routine lung cancer screening programs because of several challenges, such as perceived cost, reimbursement, lack of infrastructure and trained staff, reluctance of eligible high-risk individuals, as well as absence of well-defined guidelines.
To overcome these challenges, the experts advised having a standardized protocol for follow-up LDCT scans and considering integrated lung healthcare, such as a national screening program, to improve access to lung screening programs and subsequent care.
They also recommended enhancements to the integration of smoking cessation programs with lung cancer screening programs.
High proportion of non-smoker lung cancer patients in Asia
The experts concurred that it is essential to support high-risk patients’ access to screening procedures regardless of their smoking status by taking demographic and genetic factors into account.
They noted that, while smoking is the leading risk factor, lung cancer among never-smokers accounts for a substantial proportion of cases, especially among Asian women.
Studies have shown that compared to Europe and North America, Asia has a higher percentage of lung cancer patients who do not smoke.
In Asia, non-smokers are also more likely to receive an early diagnosis of lung cancer compared to current and former smokers.
The experts emphasized that presenting country-specific data on risk factors for never-smokers, such as age, family history of lung cancer, history of other cancers, exposure to second-hand smoke, and indoor and outdoor air pollution, could also help win government support for the establishment of lung cancer screening programs locally.